Introduction
More than 300 delegates and 36 speakers, representing Europe, America, the Middle East, Canada, Africa, Asia and Australia, convened in Berlin, Germany, in March 2015 for Smith & Nephew’s 6th International Negative Pressure Wound Therapy (NPWT) Expert Meeting. This meeting report focuses on the cardiothoracic surgery workstream discussed at the meeting.
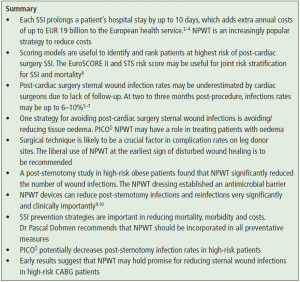
Isolated coronary artery bypass graft (CABG) surgery carries a risk of surgical-site infection (SSI) of around 3%.1 Each SSI prolongs the patient’s hospital stay by up to 10 days, which adds extra costs of up to EUR 19 billion to the European health service.2–4 Cardiac surgeons probably underestimate post-cardiac surgery sternal wound infection rates because of a lack of follow-up. At two to three months post-procedure, infection rates may be up to 6–10%.5–7
Scoring models are useful for identifying and ranking those patients who are at the highest risk of post-cardiac surgery SSI. The EuroSCORE II and Society of Thoracic Surgeons (STS) risk score may be useful for joint risk stratification for SSI and mortality.8 SSI prevention strategies are important in reducing mortality, morbidity and costs. One strategy for reducing post-cardiac surgery sternal wound infections is avoiding/reducing tissue oedema, and PICO◊ NPWT may have a role in treating patients with oedema.
Early results suggest that NPWT may hold promise for reducing sternal wound infections in high-risk CABG patients. Dr Pascal Dohmen recommended that NPWT should be incorporated in all preventative measures.
The liberal use of NPWT at the earliest sign of disturbed wound healing is to be recommended. NPWT devices can reduce post-sternotomy infections and reinfections very significantly and clinically importantly. A post-sternotomy study in high-risk obese patients found that NPWT significantly reduced the number of wound infections.9,10
Sternal complications after cardiac surgery: incidence and risk factors
The number of cardiac operations started to increase in the mid-1960s with CABG surgery, and has continued to increase in popularity ever since. The midline sternotomy is ‘easy to perform,’ well tolerated by most patients and complications are rare, Dr Richard Ingemansson said. But when complications arise they are serious. He was setting the background to his talk about sternal complications of open-heart surgery and the identified risk factors.
The main complications are:
- Deep sternal wound infection (mediastinitis) – the complication everyone fears and which kills people
- Superficial wound infection, which has no mortality risk in itself, but which, if left untreated, can become mediastinitis
- Sternal dehiscence, which is highly associated with a higher body mass index (BMI)
- Pseudoarthrosis
- Sternal pain
- Subxiphoid hernia.
Risk factors for sternal infection can be divided into pre-, peri- and postoperative or major, intermediate and minor. Preoperative risk factors are well recognised and include obesity, renal insufficiency, dialysis, diabetes mellitus (diet, oral therapy, insulin and level of HbA1c control), chronic obstructive pulmonary disease and smoking. Peri- and postoperative risk factors include the use of internal mammary artery graft (as well as preparation technique), surgical reoperation, prolonged mechanical ventilation, post-operative bleeding, extensive use of electrocautery and the use of bone wax.
Major risk factors include very low (below 18) or very high (40) BMI and insulin-dependent diabetes; intermediate factors include bilateral mammarian arteries and radiotherapy; minor factors include female gender and peripheral vascular disease.
When trying to identify risks for specific patients, the Jones Classification11 gives more information and is helpful in its classifications ranging from 1a (superficial, subcutaneous tissue dehiscence) to 3b (deep, with exposed bone and septicaemia).11
Pain after cardiac surgery is fairly common (around 28%), but severe pain is only reported in around 1% of patients.12
‘Major risk factors include very low (below 18) or very high (40) BMI and insulin- dependent diabetes; intermediate factors include bilateral mammarian arteries and radiotherapy; minor factors include female gender and peripheral vascular disease.’
Dr Richard Ingemansson
Surgical-site infections after cardiac surgery: risk score systems
Dr Johan Nilsson detailed various efforts to stratify risk: to identify and rank the patients at highest risk of developing SSIs after cardiac surgery, in an effort to optimise medical care and make maximum use of limited resources.
Risk scores began in 1986 with the USA Health Care Financing Administration’s (now known as the Centers for Medicare and Medicaid Services, CMS) publication of mortality statistics for open-heart surgery, based on ranking all cardiothoracic units on a quality-control of 30-day mortality. Since then, numerous risk score systems have been developed. The Cardiac Risk Score, from an article published by Dr Nilsson in 2006, is a synopsis of original data of 19 risk score algorithms, with a received operating characteristics (ROC) system developed to compare data.13
EuroSCORE II, an online risk calculator, is one of the most cited scoring systems in thoracic surgery today. If you go online and put in your risk factors you will get a probability of 30-day mortality.
The STS has created a database of 1–2 million patients with many risk factors for all kinds of patients and developed an online STS risk calculator that can give a percentage for risk of developing complications including renal failure, infection and stroke.
The Northern New England Cardiovascular Disease Study Group has developed a similar risk model but added a scoring model to predict mediastinitis. One of the largest, perhaps one of the first, specific scoring systems for cardiac infections was by Dr Vance Fowler,14 who used the STS database and collected information from over 300 000 coronary bypass and major infection patients to build a site infection scoring model. However, this study did not investigate all patients undergoing cardiac surgery; it focused only on those under- going CABG and did not investigate those with valves.
The statistics need to be understood in order to evaluate the different risk-scoring models: data split – the model cannot be validated on the same data set as the one on which it was developed. You must consider: internal, external and temporal validation; performance measurement – calibration (Hosmer-Lemeshow) and discrimination (ROC); and derivation and validation – does it say anything about which patient will get this complication? Ask how they performed the variable selection. It is important to know what the model was developed for: one for CABG is not appropriate for valve surgery.
One study that examined the success of existing risk scores in predicting sternal wound infection following CABG surgery concluded that EuroSCORE II and the STS risk score can be used for joint risk stratification for SSI and mortality.8
There needs to be more use of artificial intelligence and more modern risk scoring machinery in the future, such as the newly developed survival algorithm for heart transplantation (International Heart Transplantation Survival Algorithm; IHTSA).15
‘The Northern New England Cardiovascular Disease Study Group has developed a similar risk model but added a scoring model to predict mediastinitis. One of the largest, perhaps one of the first, specific scoring systems for cardiac infections was by Dr Vance Fowler,11 who used the STS database and collected information from over 300 000 patients to build a site infection scoring model.’
Dr Johan Nilsson
‘One study that examined the success of existing risk scores in predicting sternal wound infection following CABG surgery concluded that EuroSCORE II and the STS risk score can be used for joint risk stratification for SSI and mortality.8’
Dr Johan Nilsson
Strategies to reduce incisional complications after cardiac surgery
Dr Orjan Friberg outlined his personal strategies to reduce incisional complications after cardiac surgery. Cardiac surgeons often report a 1–2% rate for sternal wound infection, but that is the tip of the iceberg: the total is between 5% and 10%.
Several studies support his conclusion about the incidence of postoperative cardiac surgery wound infections.5–7 The underestimates are due to lack of follow-up: at one month, the rate is around 5–8% and by two to three months it increases to 6–10%.7
Microbiologists have found that coagulase-negative staphylococci (CoNS) are the most common bacteria: they are always present on the skin and often contaminate the sternal wound. Staphylococcus aureus, often found in the nose, may be on the patient, but should never be on the skin or in the wound.16 Gram-negative bacteria should never be present on the skin or in the wound, but can enter postoperatively through intravenous lines or catheters.17
One Swedish study showed that 89% of cardiac patients grew bacteria from the sub- cutaneous sternal tissue and 98% of patients showed bacterial growth on the surrounding skin at the end of the operation.18
There are different mechanisms to counter the different risks. To avoid contamination with the virulent bacteria (S. aureus and gram negatives), which lead to mediastinitis and septicaemia, it is vital to improve hygiene and kill those bacteria with antibiotic prophylaxis before they can cause problems. With the less virulent microbes (CoNS and Propionibacterium acnes), we should reduce contamination and optimise wound healing because we co-exist with these bacteria when there is no wound. But when there is, even the less virulent microbes, if neglected, can lead to mediastinitis.
Antibiotic prophylaxis has been shown to reduce the wound infection rate to about one-fifth compared with placebo.19 One study recommends second- or third- generation cephalosporins for cardiac surgery prophylaxis,20 although cloxacillin might be a sufficient alternative. The prophylaxis should be administered for not less than 24 hours and not more than 48 hours. The first dose must be given immediately before skin incision and repeated during surgery. Glycopeptides are less effective antibiotics than beta- lactams21 and are associated with increased renal failure.22
Recent meta-analysis shows a significant reduction in the risk of sternal wound infections after cardiac surgery with the use of gentamicin-collagen sponge,23 so maybe it is time to adopt this approach.
Dr Friberg’s recommended strategies were:
- Avoid ischaemia and minimise electrocautery
- Optimise glucose control – never let postoperative blood sugar levels get too high
- Maintain an optimal temperature
- Avoid or reduce tissue oedema by exercising a very restricted fluid policy intraoperatively
- Use the NPWT system PICO◊ for treating patients with oedema.
Orthopaedic surgeons’ studies have shown the importance of a rigid sternal fixation: with a contaminated fracture, fix it very rigidly with plate and screws, and it takes a high bacterial population before it becomes infected, but with a tiny amount of movement in the fracture it takes very few bacteria before there is a clinical infection.24 Put in extra wires, said Dr Friberg.
Leg donor site infections: complication rates and strategies to minimise them
Dr Friberg talked about complication rates in leg donor site infections and ways to minimise them. By definition, the vein is harvested subcutaneously, so surgeons are never deep and all wounds on the site are therefore super- ficial. That does not mean they are not serious. If a doctor has prescribed an antibiotic, it is an infection.
There are three main risk factors: diabetes, female sex and obesity. Diabetic patients obviously have a poor circulation, female leg skin often seems to be very thin, obesity is a factor in all catheter-borne infections and subcutaneous tissue is less well able to heal than muscular tissue. There are few studies on strategies to reduce infection in leg donor sites. One solution could be to change the surgical technique: endoscopic vein harvest is increasingly popular, especially in the USA but also in Europe. It was developed to eliminate the need for the long incisions associated with open harvesting, and to decrease the risk of wound infection and other complications, as well as reduce postoperative pain and length of hospital stay, among other things. However, a retrospective post hoc analysis of a high-quality large study showed that endoscopic vein harvest is associated with vein-graft failure and is linked with worse clinical outcomes and higher mortality than open harvesting.25 The method of graft harvesting was determined by the surgeon and randomised trials are needed to further evaluate the safety and effectiveness of the harvesting technique.
In Dr Friberg’s opinion, surgical technique is probably a very crucial factor in the complication rates on leg donor sites, but there are no published studies. More prospective randomised trials are needed in the use of endoscopic vein harvesting, and into triclosan sutures and microbial sealant. The liberal use of NPWT at the earliest sign of disturbed wound healing is to be recommended and further studies are needed to investigate its role as a prophylaxis.
There are three main risk factors: diabetes, female sex and obesity. Diabetic patients obviously have a poor circulation, female leg skin often seems to be very thin, obesity is a factor in all catheter-borne infections and subcutaneous tissue is less well able to heal than muscular tissue.’
Dr Orjan Friberg
‘Surgical technique is probably a very crucial factor in the complication rates on leg donor sites…The liberal use of NPWT at the earliest sign of disturbed wound healing is to be recommended.’
Dr Orjan Friberg
Effect of surgical incision management on wound infections in a post-sternotomy patient population
Dr Onnen Grauhan talked about the effect of surgical incision management on post-sternotomy wound infection patients. He began with the cause of wound infections because, he said, that is where the notion of treatment or prevention begins. He moved on to the concept of prophylactic NPWT, then to his clinical experience with the problem.
A study of deep sternal wound infections or mediastinitis26 found that more than two-thirds of all the infections had the same aetiology: breakdown of skin suture, especially in obese patients. Only a small part is caused by perioperative contamination. The key event in most infections seems to be the breakdown of skin suture and consequent seepage of skin flora into the sternum.
A second important study7 alerts us to the delay between removing the sutures, believing all is clear, and the appearance of infections. Most infections occur later (up to 90 days later) and follow-up is vital. Dr Grauhan’s study with ‘high-risk’ patients ran from April 2010 to October 2011;9 an ‘all-comers’ study ran from September to October 2013.10 His multi-centre trial started in April 2014 and is ongoing.
The ‘high-risk’ patient study was a two- arm prospective study of 150 obese patients (BMI ≥30kg/m2). The primary endpoint was wound infection requiring surgical revision within 90 days. There were 75 in the NPWT foam dressing (PrevenaTM) group and 75 in the control (conventional wound dressing) group. The trial found that there were 12 infections in the control group and three in the NPWT group after 90 days.9
There is a significant difference in all infections, but the concept was to avoid infections by skin flora and there was only one patient infection (a small dehiscence) in the NPWT group, compared with 10 patients in the control group, a highly significant and clinically important difference (p=0.0090; 95% CI 1.42–91.36). When the NPWT dressing was removed, the incision was already closed/healed.9
The study found that prophylactic NPWT over clean, closed incisions for the first six to seven postoperative days significantly reduces the incidence of wound infection after median sternotomy in the high-risk group of obese patients.9
His prospective ‘all-comers’ cohort trial (September to October 2013) included 237 patients with sternotomy and a retrospective ‘historical’ control group of 3508 patients (January 2008 to December 2009). The primary endpoint was wound infection requiring surgical revision.10
The conclusion from both studies was that the very high infection rate for high-risk patients can be reduced by NPWT from 16% to 4%;9 and in all-comers from 3.4% to 1.3% (Figure 1).10 Dr Grauhan’s verdict: ‘We believe these devices can reduce the infections and reinfections very significantly and clinically importantly. We believe it might be useful to have these devices, not only for a week but for 10–12 days to prevent, even in badly healing wounds, these infections.’
We believe these [NPWT] devices can reduce the infections and reinfections very significantly and clinically importantly. We believe it might be useful to have these devices, not only for a week but for 10–12 days to prevent, even in badly healing wounds, these infections.’
Dr Onnen Grauhan
Prophylactic NPWT can reduce very high infection rates in high-risk obese patients using conventional dressings from 16% to 4%, and in ‘all-comers’ from 3.4% to 1.3%.9’
Dr Onnen Grauhan
Costs associated with surgical-site infections after cardiac surgery
Some preventative strategies recommended by Dr Pascal Dohmen for avoiding SSIs include:
- Standardisation of surgery allows reduced operative time, but he cautions not to discharge patients too early
- Minimally invasive surgery – do not make a big incision unless it is necessary
- Avoid bone wax
- Change gown and gloves more often.
SSI prevention strategies are vital for reducing mortality, morbidity and costs. The risk of SSI for future patients will further increase, and there should be screening and treatment for methicillin-resistant/-sensitive S. aureus.27 NPWT should be incorporated in all preventative measures.
‘NPWT should be incorporated in all preventative measures.’
Dr Pascal Dohmen
Groin surgical incisions: specific challenges and initial evidence on NPWT
Dr Stefan Acosta described the specific challenges associated with groin surgical incisions and revealed the early results of a study into the use of NPWT. There is a high incidence of wound infection after vascular surgery in the groin, which is not surprising given its proximity to the genital area and cloacal system.
His department has kept a wound surveillance registry for SSIs since 2005 and in 2012–13, it conducted a study of SSI following infra-inguinal groin incision for vascular surgery after changing their antibiotic prophylaxis regimen from cloxacillin to sulfamethoxazole / trimethoprim. The two groups were equal in terms of endovascular procedures and in other risk factors. There was a very high wound infection rate of SSI on cloxacillin, but no significant difference after changing the antibiotic prophylactic regimen.
Risk factors identified for SSI in the groin after vascular surgery for patients, include those identified by other surgical procedures, such as diabetes, obesity, smoking, prior incision site irradiation/operation. Procedure-related risks include those from synthetic grafts and a 30–40% rate for infection after reoperation for bleeding.
Morbidity and mortality rates of peri-vascular SSI in the groin are high: amputation levels of 10–30%, sometimes directly related to infection in the groin, sometimes to ischaemia in the leg, and mortality of 10–30% in patients who often have high rates of comorbidities.
Management ranges from debridement, surgical revision, antibiotics and graft preservation to graft removal and leg amputation to save the patient’s life. Some patients are only fit for conservative treatment, whereupon NPWT is applied, changed three times a week and sometimes, after some months, real wound healing is achieved.
The centre recognised its need to reduce its very high rate of wound infection after vascular surgery and to improve prevention, so in November 2013 began a controlled trial, randomising between the PICO◊ and standard wound dressing. A total of 70% of patients had bilateral groin incisions, which made it a particularly interesting study.
So far, they have evaluated 81 patients with a three-month follow-up. There are 64 groin incisions in the NPWT group and 63 in the control group. Preliminary results show the overall groin infection rate dropped to 11.1% (9/81), compared to the centre’s 2013 groin SSI rate of 22.5% (p=0.085). ‘Something dramatic has happened, whether it’s PICO◊ or surgeon awareness, I don’t know. It looks promising, but numbers are small at this point.’
‘Some patients are only fit for conservative treatment, whereupon NPWT is applied, changed three times a week and sometimes, after some months, real wound healing is achieved.’
Dr Stefan Acosta
NPWT to reduce the incidence of incisional complications after sternotomy: a randomised, controlled study
Dr Carlos Velasco explained the background to his randomised controlled study into the effect of using NPWT to reduce the incidence of incisional complications after sternotomy, and revealed the study’s preliminary results. Although infrequent, sternal wound complications following median sternotomy remain a challenge, with life-threatening consequences for the patient and high costs for healthcare providers.
NPWT has become widely used in the past 20 years, but Dr Velasco and his colleagues wanted to explore the less well-documented use of NPWT as a preventative strategy on closed surgical incisions. They designed an ongoing study (CHUAC) to compare PICO◊ and conventional sterile dry-wound dressing in a high-risk group, with special regard to wound complications and infections, and evaluate the economic costs of PICO◊. Primary outcomes include wound infection and wound dehiscence. Secondary outcomes are hospital costs and length of stay.
Patients included in the study were at high risk of developing wound infection (with multiple comorbidities), aged over 18, and at the hospital for isolated or combined myocardial revascularisation surgery. They were excluded if they were receiving immunosuppressive therapy, had thoracic skin disease and tape allergies, or if they could not otherwise tolerate NPWT. The Centers for Disease Control and Prevention (CDC) classification of SSI was used (infection occurring within 30 days post-surgery or within one year with implant).
Out of 1252 patients who were evaluated, 362 at high risk for sternal infection (according to EuroSCORE and Fowler score) agreed to participate. They were randomised prior to surgery into two groups: 187 PICO◊ (placement of the PICO◊ system along the line of closure in the operating room); 175 controls (standard dry sterile dressing consisting of a non-adhesive silicone layer).
So far, trends show a reduction in the number of infections in the PICO◊ group (11 versus 19) and their severity; a shorter length of stay, less need of NPWT and a less expensive antibiotherapy treatment, which reflects less aggressive infections in the PICO◊ group. There is evidence that the costs of treatment in the control group were twice that of the PICO◊ group due to higher rates of infection and higher treatment costs.
Although there is still no evidence of a significant difference between the two groups, there is a trend showing that PICO◊ seems to act as a mechanical barrier to decrease infection in the groups where it was used. There will be a statistical analysis to assess results at the end of the follow-up period. As sternal wound infection is an infrequent complication, a multi-centre clinical trial would be valuable to provide stronger evidence.
‘There is a trend showing that PICO◊ seems to act as a mechanical barrier to decrease infection in the groups where it was used.’
Dr Carlos Velasco
Use of NPWT to prevent postsurgical complications on mammary bypass patients: clinical experience
Dr Martin Oberhoffer talked about the choice of bypass graft and its consequences before unveiling the preliminary results of his study with NPWT (PICO◊). About 60% of the 100 000 operations performed annually in 79 German cardiothoracic centres are bypass and combined operations. The choice of bypass graft has long-term consequences. It is known that 10 years after CABG, 90–95% of cases are patent and disease free. There is a lack of data on long-term patency rates on radial artery grafts, but we know it is only suitable for coronary artery stenosis exceeding 75–85%, depending on which literature you read. We also know that 75% of vein conduits are blocked or severely diseased 10 years after CABG.
Graft failure leads to a high risk of recurrent angina, late myocardial infarction and a need for further interventions. This means that after 10–15 years, one-third of the patients might need redo CABG, which is associated with a high risk of death.
Living with left internal mammarian (thoracic) artery (LIMA/LITA) and vein grafts may seem tolerable, but the literature provides different information. One study looking at the effect of bilateral internal mammarian (thoracic) artery (BIMA/BITA) grafting on 20-year survival concluded that it produces improved survival compared with single internal thoracic artery grafting during the second postoperative decade, and the magnitude of that benefit increases through 20 postoperative years.28
Another study, with more than 3500 patients, investigated the use of LIMA/ LITA versus BIMA/BITA and identified that BITA grafting confers a long-term survival advantage regardless and should be performed whenever suitable.29 The most recent meta-analysis compared LIMA versus BIMA (BITA) in 2014 and included 20 observational studies, a multitude of authors from different years and an analysis of more than 70 000 patients. It concluded that BITA grafting seems to significantly reduce long-term mortality.30
In April 2014, Dr Oberhoffer and his colleagues started a study with the NPWT (PICO◊) system in a high-risk group of patients undergoing total arterial revascularisation (BIMA) and combined procedures using BIMA. They collected data on pre-, intra- and postoperative parameters, evaluated the STS mediastinitis score and documented sternal wound complications regarding the outcome: secondary closure/plastic surgical intervention.
Preliminary results revealed that the NPWT (PICO◊) system for reducing sternal wound infections in high-risk CABG patients is ‘promising’. Cost-effectiveness calculations might justify its clinical use, but the number of patients is too small yet to detect significant effects. Continuous documentation of a further 300, and up to 500 patients is ongoing. A randomised controlled trial would be welcome to clarify whether or not significant differences occur.
‘Preliminary results with the NPWT (PICO◊) system for reducing sternal wound infections in high-risk CABG patients are promising.’
Dr Martin Oberhoffer
Conclusions
Preventing SSIs is key to substantial savings in any surgical service and will ultimately reduce the length of a patient’s stay in hospital. Patients can be ranked in order of their risk of contracting an SSI postsurgery, and it is vital that surgeons maintain a good grasp of statistics in order to evaluate the different models that have been developed. A lack of follow-up of post-cardiac surgery patients is believed to have led to the underestimation of SSI rates in this population. Indeed, it is estimated that rates of superficial wound infection could be between 6% and 10%.5–7 Avoiding or reducing tissue oedema is a strategy for avoiding post-cardiac surgery sternal wound infections, and it is thought that PICO◊ NPWT may have a role in treating oedema patients. In patients with leg donor sites, surgical technique is key to reducing complication rates and use of NPWT at the earliest sign of disturbed wound healing is recommended. Use of NPWT (PrevenaTM) was found to significantly reduce the number of wound infections in a population of post-sternotomy obese (high-risk) patients.9 Use of NPWT devices may reduce morbidity, mortality and costs. It is possible that PICO◊ might also act to prevent infections postsurgery, with several ongoing studies in progress.
Summary
References
- Dohmen PM, Gabbieri D, Weymann A, et al. Reduction in surgical site infection in patients treated with microbial sealant prior to coronary artery bypass graft surgery: a case-control study. J Hosp Infect 2009;72:119–26.
- Leaper DJ, van Goor H, Reilly J, et al. Surgical site infection – a European perspective of incidence and economic burden. Int Wound J 2004;1:247–73.
- Ronveaux O, Mertens R, Dupont Y, et al. Surgical wound infection surveillance: results from the Belgian hospital network. Acta Chir Belg 1996;96:3–10.
- Plowman R, Graves N, Griffin MAS, et al. The rate and cost of hospital-acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden imposed. J Hosp Infect 2001;47:198–209.
- Risnes I, Abdelnoor M, Lundblad R, et al. Sternal wound closure in patients undergoing open-heart surgery: a prospective randomized study comparing intracutaneous and zipper techniques. Eur J Cardiothorac Surg 2002;22:271–7.
- Dhadwai K, Al-Ruzzeh S, Athanasiou T, et al. Comparison of clinical and economic outcomes of two antibiotic prophylaxis regimens for sternal wound infection in high-risk patients following coronary artery bypass grafting surgery: a prospective randomised double-blind controlled trial. Heart 2007;93:1126–33.
- Jonkers D, Elenbaas T, Terporten P, et al. Prevalence of 90-days postoperative wound infections after cardiac surgery. Eur J Cardiothorac Surg 2003;23:97–102.
- Paul M, Raz A, Leibovici L, et al. Sternal wound infection after coronary artery bypass graft surgery: validation of existing risk scores. J Thorac Cardiovasc Surg 2007;133:397–403.
- Grauhan O, Navasardyan A, Hofmann M, et al. Prevention of poststernotomy wound infections in obese patients by negative pressure wound therapy. J Thorac Cardiovasc Surg 2013;145:1387–92.
- Grauhan O, Navasardyan A, Tutkun B, et al. Effect of surgical incision management on wound infections in a poststernotomy patient population. Int Wound J 2014;11(Suppl 1):6–9.
- Jones G, Jurkiewicz MJ, Bostwick J, et al. Management of the infected median sternotomy wound with muscle flaps. The Emory 20-year experience. Ann Surg 1997;225:766–78.
- Meyerson J, Thelin S, Gordh T, Karlsten R. The incidence of chronic post-sternotomy pain after cardiac surgery – a prospective study. Acta Anaesthesiol Scand 2001;45:940–4.
- Nilsson J, Algotsson L, Höglund P, et al. Comparison of 19 pre-operative risk stratifica- tion models in open-heart surgery. Eur Heart J 2006;27:867–74.
- Fowler Jr VG, O’Brien SM, Muhibaier LH, et al. Surgery for coronary artery disease. Clinical predictors of major infections after cardiac surgery. Circulation 2005;112:1358–65.
- Nilsson J, Ohlsson M, Höglund P, et al. The International Heart Transplant Survival Algorithm (IHTSA): a new model to improve organ sharing and survival. PLoS ONE 2015;10:e0118644.
- Stahl E, Tammelin A, Bergstrom R, et al. Sternal wound complications – incidence, microbiology and risk factors. Eur J Cardio Surg 1997;11:1146–53.
- Peleg AY, Hooper DC. Hospital-acquired infections due to gram-negative bacteria. N Engl J Med 2010;362:1804–13.
- Kühme T, Isaksson B, Dahlin L-G. Wound contamination in cardiac surgery. A system- atic quantitative and qualitative study of bacterial growth in sternal wounds in cardiac surgery patients. APMIS 2007;115:1001–7.
- Kreter B, Woods M. Antibiotic prophylaxis for cardiothoracic operations. Meta-analysis of thirty years of clinical trials. J Thoracic Cardiovasc Surgery 1992;104:590–9.
- Lador A, Nasir H, Mansur N, et al. Antibiotic prophylaxis in cardiac surgery: systematic review and meta-analysis. J Antimicrob Chemother 2012;67:541–50.
- Bolon MK, Morlote M, Weber SG, et al. Glycopeptides are no more effective than beta-lactam agents for prevention of surgical site infection after cardiac surgery: a meta- analysis. Clin Infect Dis 2004;38:1357–63.
- Olsson DP, Holzmann MJ, Sartipy U. Antibiotic prophylaxis by teicoplanin and risk of acute kidney injury in cardiac surgery. J Cardiothorac Vasc Anesth 2015;29:626–31.
- Kowalewski M, Pawliszak W, Zaborowska K, et al. Gentamicin-collagen sponge reduces the risk of sternal wound infections after heart surgery: meta analysis. J Thorac Cardiovasc Surg 2015;149:1631–40.e6.
- Friberg O, Dahlin LG, Söderquist B, et al. Influence of more than six sternal fixation wires on the incidence of deep sternal wound infection. Thorac Cardiovasc Surg 2006;54:468–73.
- Lopes RD, Hafley GE, Allen KB, et al. Endoscopic versus open vein graft harvesting in coronary-artery bypass surgery. New Engl J Med 2009;361:235–44.
- Gårdlund B, Bitkover CY, Vaage J. Postoperative mediastinitis in cardiac surgery – microbiology and pathogenesis. Eur J Cardiothorac Surg 2002;21:825–30.
- van Rijen MML, Bode LGM, Baak DA, et al. Reduced costs for Staphylococcus aureus carriers treated prophylactically with mupirocin and chlorhexidine in cardio- thoracic and orthopaedic surgery. PLoS ONE 2012;7:e43065.
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004;78:2005–14.
- Puskas JD, Sadiq A, Vassiliades TA, et al. Bilateral internal thoracic artery grafting is associated with significantly improved long- term survival, even among diabetic patients. Ann Thorac Surg 2012;94:710–6.
- Takagi H, Goto SN, Watanabe T, et al. A meta-analysis of adjusted hazard ratios from 20 observational studies of bilateral versus single internal thoracic artery coronary artery bypass grafting. J Thorac Cardiovasc Surg 2014;148:1282–90.